How the opioid epidemic became America’s worst drug crisis ever, in 15 maps and charts
Drug overdoses now kill more Americans than HIV/AIDS did at its peak. These maps and charts tell the story.
Updated byVideo
America is in the middle of its deadliest drug crisis ever.
With all the other news going on, it can be easy to lose
track of this fact. But it’s true: In 2015, more than 52,000 people died
of drug overdoses, nearly two-thirds of which were linked to opioids
like Percocet, OxyContin, heroin, and fentanyl. That’s more drug
overdose deaths than any other period in US history — even more than
past heroin epidemics, the crack epidemic, or the recent meth epidemic.
And the preliminary data we have from 2016 suggests that the epidemic
may have gotten worse since 2015.
This situation did not develop overnight, but it has
quickly become one of the biggest public health crises facing America.
To understand how and why, I’ve put together a series of maps and charts
that show the key elements of the epidemic — from its start through legal painkillers prescribed in droves by doctors to the recent rise of the highly potent opioid fentanyl.
1) Drug overdoses now kill more people than gun homicides and car crashes combined
To understand just how bad the opioid epidemic has
gotten, consider these statistics: Drug overdoses in 2015 were linked to
more deaths than car crashes or guns, and in fact killed more people
than car crashes and gun homicides combined. Drug overdoses in
2015 also killed more people in the US than HIV/AIDS did during its peak
in 1995. So just as HIV/AIDS lives in the American mind as a horrible
epidemic, the current opioid epidemic should too.
2) Drug, painkiller, heroin, and other opioid overdose deaths are still on the rise
It took years of increasing deaths to get to this point,
but the opioid epidemic has only gotten worse over time. The result is
horrifying: Between 1999 and 2015, more than 560,000 people in the US
died to drug overdoses — a death toll larger than the entire population
of Atlanta.
The epidemic has by and large been caused by the rise in
opioid overdose deaths. First, opioid painkiller overdoses began to
rise, as doctors began to fill out a record number of prescriptions for
the drugs in an attempt to treat patients’ pain conditions. Then, people
hooked on painkillers began to move over to heroin as they or their
sources of drugs lost their prescriptions. And recently, more people
have begun moving to fentanyl, an opioid that’s even more potent and
cheaper than heroin. The result is a deadly epidemic that so far shows
no signs of slowing down.
3) Opioid overdoses are one reason US life expectancy declined for the first time in decades
In 2015, US life expectancy dropped for the first time in decades. There are many causes behind the drop, including rising rates of diabetes, obesity, and suicide. But a big reason for the decrease was the rise in alcohol poisonings and drug overdoses.
4) The epidemic is much worse in some states than others
Not every state in America has been equally impacted by
the opioid epidemic. States like West Virginia, New Hampshire, Rhode
Island, and Ohio have been hit particularly hard, suffering far more
deaths than even their neighbors on an annual basis. And the epidemic
has generally been concentrated along the Rust Belt and New England —
due in large part, it seems, to the enormous number of painkiller
prescriptions that doctors doled out in those areas.
5) By and large, the drug overdose epidemic has hit white Americans the hardest
The drug overdose epidemic hasn’t hit people of all
racial groups equally either, with white Americans suffering far more
overdose deaths than their black and Latino peers. As the chart above
shows, this is a shift from before the 2000s, when past drug crises
tended to hit black, urban communities much harder.
One reason for the disparity may, ironically, be racism against nonwhite Americans. Studies
show that doctors are more reluctant to prescribe painkillers to
minorities, because doctors mistakenly believe that minority patients
feel less pain or are more likely to misuse and sell the drugs. In a
perverse way, this shielded minority patients from the tsunami of opioid
painkiller prescriptions that got white Americans hooked on opioids and
led to a wave of deadly overdoses.
6) Americans consume more opioids than any other country
This is perhaps the most important chart to understand
why America in particular is suffering from the epidemic: Simply put,
the US consumes far more opioid painkillers than any other
country in the world. When a country collectively consumes more of a
deadly, addictive drug, it’s obviously going to have more deaths as a
result of those drugs.
7) In some states, doctors have filled out more painkiller prescriptions than there are people
So why do Americans consume so many opioids? In short,
it’s because doctors have prescribed a lot of them. Starting in the
1980s and ’90s, doctors were under pressure to take pain more seriously.
There was some good reason for that: About 100 million Americans suffer
from chronic pain, according to a 2011 report
from the Institute of Medicine. So doctors — under pressure from drug
companies, medical organizations, government agencies, and pain patient
advocates — resorted to opioids.
The result: In 2012, US physicians wrote 259 million prescriptions for opioid painkillers — enough to give a bottle of pills to every adult in the country.
And these pills didn’t just end up in patients’ hands; they also
proliferated to black markets, were shared among friends and family,
landed in the hands of teens who rummaged through parents’ medicine
cabinets, and so on.
8) Drug companies have made a lot of money from opioids
One of the undeniable contributors to the opioid epidemic
is drug companies. Seeing the demand for doctors to take pain more
seriously, drug companies pitched newer products like OxyContin as the
big medical solution. The marketing was extremely misleading, often
presenting these drugs as safer and more effective than other
painkillers and opioids on the market — when these drugs were in fact
extremely addictive and dangerous.
Ultimately, some drug companies would pay for their misleading marketing. Purdue Pharma, producer of OxyContin, in 2007 paid hundreds of millions of dollars in fines for its false claims. And Purdue and other opioid producers remain in legal battles over the drugs to this day.
9) At the same time, Americans report greater levels of pain
Despite the increase in painkiller prescriptions, studies
show that Americans generally report higher levels of chronic pain than
they did before the epidemic started.
This gets to a crucial point in the opioid epidemic:
Despite drug companies’ marketing, opioid painkillers aren’t an
effective treatment for chronic pain. There’s simply no good scientific evidence that painkillers can actually treat long-term pain as patients grow tolerant of the painkilling effects, but there’s plenty of evidence that prolonged use can result in very bad complications, including a higher risk of addiction, overdose, and death.
Yet painkillers, due to how they work, can actually trick
patients into believing that the drugs are effective for chronic pain.
As Stanford psychiatrist Anna Lembke, author of Drug Dealer, MD, recently explained:
It’s absolutely true that if you were to get opioids for your pain, it would be like a magical cure for about a month or maybe two. But after a while, there’s a very high likelihood that they would stop working. And then you would have two problems: You would have your pain, and you would be dependent on this drug and experience painful withdrawal if you try to get off [opioids].
So after prolonged use, some patients who try to stop
taking opioids will feel a sudden surge of pain. They’ll likely think
the pain they’re feeling is their chronic pain coming back in full force
now that the painkillers are gone. In reality, the opioids have likely
stopped working on the original chronic pain due to tolerance, and the
surge of pain is an entirely new pain from drug dependence withdrawal.
Only by slowly weaning themselves off opioids can they permanently stop
this new withdrawal-induced pain.
There’s also evidence that opioids can make pain worse. Opioids might make people more sensitive to pain. They might weaken the bones.
And they might get people to behave in ways that expose
them to greater injury, which of course would lead to far more pain.
Lembke gave an example of someone popping extra pills to let them do
more yard work: “If you take additional opioids, you can’t hear the
signals from your body about what you shouldn’t be doing, and then maybe
you’re going to do some long-term damage above what’s already been
done.”
10) Painkillers are often prescribed for long periods of time, even though there’s no evidence they effectively treat chronic pain
Despite the lack of evidence for opioids’ effectiveness
in treating chronic pain, doctors have resorted to prescribing the
opioids to patients for exorbitant periods of time. (I can’t even count
the number of people, from friends to family to colleagues, who have
told me that a doctor prescribed extra weeks of pills “just to be
safe.”)
This, it turns out, is extremely dangerous: A recent study
from the Centers for Disease Control and Prevention revealed that the
risk of dependency increases dramatically for each day someone is
prescribed opioids. Overly long prescriptions, then, contribute to the
cycle of addiction, overdose, and death that’s spread across the US in
the past few years.
Yet if opioids aren’t the answer to chronic pain, what is? There are alternative treatments,
although these can involve more work (and money) than just taking a
pill — such as physical therapy, massage, and acupuncture. More exotic
but less tested ideas include medical marijuana and kratom.
But the reality is that, at some level, some patients
struggling with chronic pain may just have to learn to live with the
pain. This may sound cruel, but it’s something that’s asked of patients
dealing with other chronic conditions when medicine just has no good
answers. For example, a patient with heart disease might be told that
she needs to eat less or adjust her activity level — potentially ruining her interests or hobbies — to avoid a heart attack as she becomes older.
“You can’t use the pills to extend your limits. You have
to accept that there’s some things you just won’t be able to do
anymore,” Lembke told me. “People are very resistant to that idea. I
think that speaks to some of the core hope for at least Americans that
they should really be able to keep doing what they were doing in their
20s, and that somehow a doctor should be able to fix them and make that
happen, instead of accepting that maybe that’s something that they just
can’t do anymore.”
11) States are now cracking down on opioid prescriptions
As the problem with opioid painkillers continues,
different levels of government and regulatory bodies have taken steps to
restrict their use. Some states, for example, have limited how long
opioid painkillers can be prescribed. The idea is simple: After years of
letting these painkillers run amok and kill tens of thousands of
people, doctors need to be told to take a much more conservative
approach to dangerous drugs.
12) Heroin overdose deaths now kill more people than commonly prescribed painkillers
As governments and regulators cracked down on
painkillers, however, many people addicted to the drugs didn’t just stop
using. Many instead resorted to another opioid to fill their habit:
heroin. A 2014 study in JAMA Psychiatry found many painkiller users were moving on to heroin, and a 2015 CDC analysis
found people who are addicted to prescription painkillers are 40 times
more likely to be addicted to heroin. Not all painkiller users went this
way, and not all heroin users started with painkillers, but painkiller
use played a big role in leading more people to heroin.
The main reason for this: Heroin is extremely cheap in
the black market, despite law enforcement efforts for decades to push up
the price of drugs by cracking down on the illicit supply. In fact,
over the past few decades, the price of heroin in the US has
dramatically dropped — to the point that it’s not only cheaper than
opioid painkillers sold in the black market, but frequently even candy bars.
But heroin is also more potent and, therefore, deadlier
than opioid painkillers. So even though not every painkiller user went
to heroin, just enough did to cause the big spike in heroin overdose
deaths that America has seen over the past few years. So now more people
die of overdoses linked to heroin than die of overdoses linked to
commonly prescribed painkillers.
That doesn't mean cracking down on painkillers was a
mistake. It appeared to slow the rising number of painkiller deaths, and
may have prevented doctors from prescribing the drugs — or letting them
proliferate — to new generations of people who’d develop drug use
disorders. So the crackdown did lead to more heroin deaths, but it will
hopefully prevent future populations of drug users, who could have
suffered even more overdose deaths.
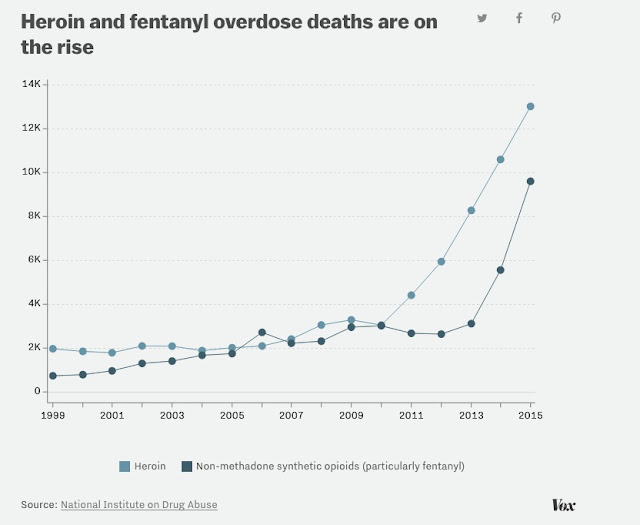
13) Fentanyl has become a growing problem as well
As if the rise in heroin deaths wasn’t bad enough, over the past few years there has been evidence of another
opioid that’s even more potent than heroin leading to more drug
overdose deaths: fentanyl. Sometimes drug users purposely seek out this
drug. But often it’s laced in other substances, like heroin and cocaine,
without the users knowing it, leading to an overdose.
The fact that the efforts to crack down on the supply of
opioid painkillers has only led people to even more dangerous drugs
hints at another lesson from the epidemic: Just cutting access to
opioids isn’t enough. As long as people are addicted, they’re going to
try to find ways to satisfy that addiction, even if it means using more
dangerous drugs.
So while cutting access to opioids might in the long term
stop the creation of new generations of people with drug use disorders,
in the shorter term the country needs to devise solutions for how to
get people to stop using drugs and how to make their drug use less
deadly and dangerous. That’s where drug treatment, including medication-assisted treatment that replaces dangerous opioid use with safer opioids like buprenorphine, and harm reduction efforts, such as clean needle exchanges, can help.
14) Anti-anxiety drugs are involved in more overdoses as well
Opioid painkillers aren’t the only legal drug that’s killing more people. Federal data shows that benzodiazepines, such as Xanax and Valium, are also increasingly involved in overdose deaths.
This speaks to another aspect of the drug overdose
epidemic: It’s not always just one drug killing people. Very often,
people use multiple drugs, from painkillers to cocaine to alcohol. This
is especially bad because different drugs can heighten other drugs’ risk
of overdose. Alcohol and benzodiazepines, for instance, are known to
compound the overdose risk of opioids.
The data speaks to this: Most benzodiazepine overdoses
have involved opioids in the past few years, as the chart above shows.
And the Centers for Disease Control and Prevention previously found that 31 percent of opioid painkiller overdose deaths in 2011 were also linked to benzodiazepines.
15) Most people who meet the definition for a drug use disorder don’t get treatment
While drug treatment may be the true solution to the
opioid epidemic, the reality is it remains inaccessible to a lot of
people. According to 2014 federal data,
at least 89 percent of people who met the definition for having a drug
use disorder didn’t get treatment. And that’s likely an underestimate:
Federal household surveys leave out incarcerated and homeless
individuals, who are more likely to have serious, untreated drug
problems.
The reasons why vary. People might not have insurance
to pay for drug treatment. If they do have insurance, their plans may
not fully cover drug treatment. And even if their plans do cover drug
treatment, there might not be enough space in treatment facilities to
take them, leading to weeks- or months-long waiting periods for care.
In general, all of this suggests that the country as a
whole needs to put more resources toward making drug treatment options
more widespread, accessible, and affordable. So far, Congress has taken
some steps to that end, including a recent $1 billion boost in drug treatment funding over two years.
But as so many people with drug use disorders struggle to get into
treatment and the opioid epidemic continues, the call will likely grow
for more action.















Thanks for posting this info. I just want to let you know that I just check out your site and I find it very interesting and informative. I can't wait to read lots of your posts. cash pay drug testing marble falls
ReplyDelete